ADHD is a diverse disorder with complex epidemiology and aetiology, which can have a significant impact on affected individuals’ lives.
What is ADHD?
Attention-deficit hyperactivity disorder (ADHD), or hyperkinetic disorder (HKD), is a diverse neurodevelopmental condition characterised by symptoms of inattention, hyperactivity and impulsivity, and can have a significant impact on affected individuals’ lives.1,2 There are two key medical classification systems used to define ADHD:
- The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders – 5th Edition (DSM-5TM) medical classification system which defines ADHD as “a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development”.1
- The International Classification of Diseases 11th Revision (ICD-11), which defines ADHD as “a persistent pattern of inattention and/or hyperactivity-impulsivity that has a direct negative impact on academic, occupational or social functioning”.2
How common is ADHD?
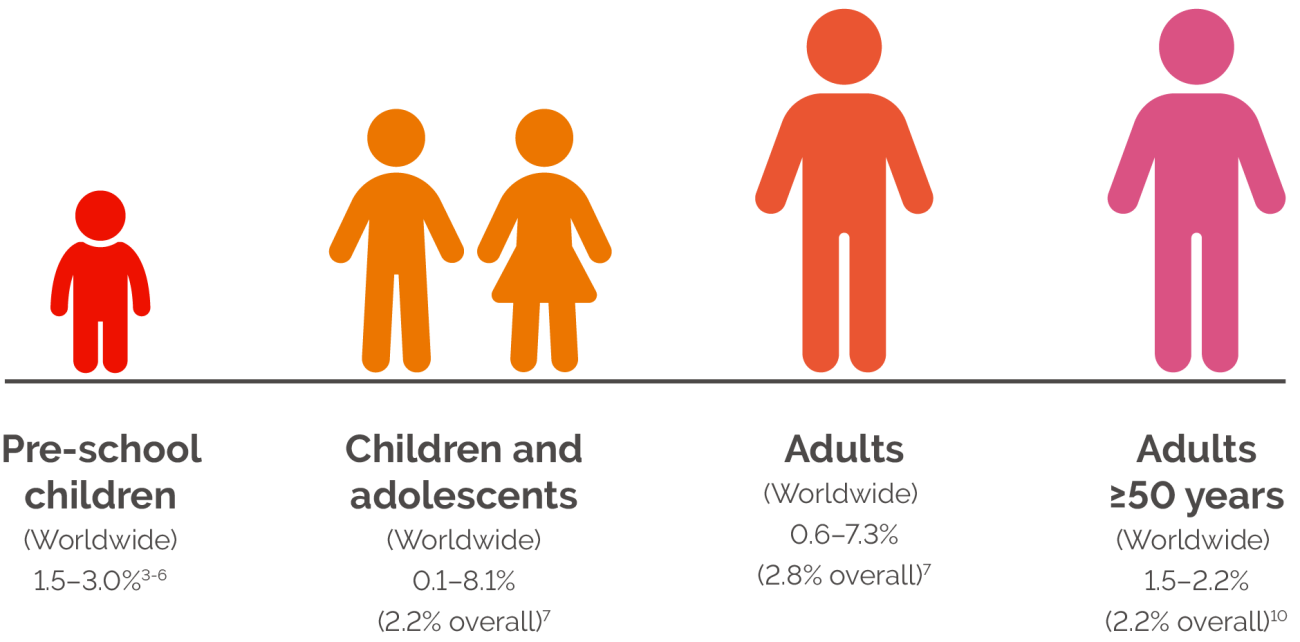
ADHD is known to persist across the lifespan and affects people of all ages. ADHD prevalence rates vary between children, adolescents and adults (Figure 1), and by gender and symptom presentation.1,3-9
UNDERSTANDING ADHD: A LIFELONG JOURNEY
FIGURE 1
SUMMARY OF ADHD PREVALENCE RATES IN DIFFERENT AGE GROUPS.
Figure developed from multiple sources.3-7,10
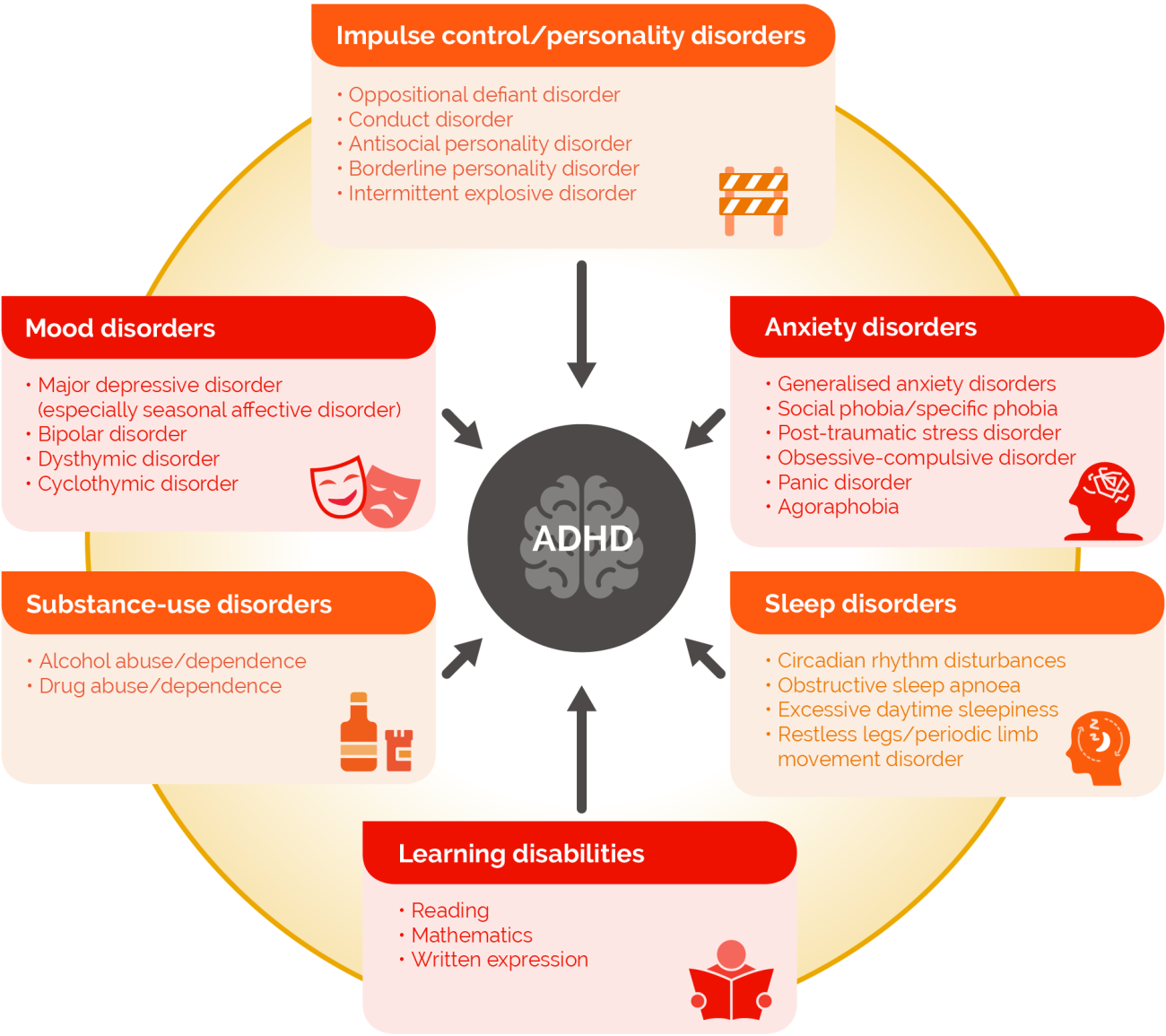
What comorbid psychiatric disorders are associated with ADHD?
The majority of adults with ADHD have a diagnosed or undiagnosed psychiatric comorbidity, which can complicate the diagnosis and treatment of ADHD (Figure 2).2,11,12
FIGURE 2
MAIN COMORBID PSYCHIATRIC DISORDERS IN ADULT ADHD.
Reproduced with permission from Kooij JJS et al. J Atten Disord 2012; 16(5 Suppl): 3S-19S.13
UNDERSTANDING ADHD: EXPLORING ASSOCIATED PSYCHIATRIC COMORBIDITIES
What causes ADHD?
The aetiology of ADHD is complex and is thought to have a neurobiological component, an underlying genetic component and be associated with several environmental risk factors, which may increase the likelihood of some ADHD symptoms.14-66
What is the impact of ADHD?
ADHD can have a significant social impact on affected individuals’ lives, causing disruption at school, work, and in relationships.67-75 Symptoms of ADHD may also increase risk-taking behaviour.67,76,77 Consequently, the quality of life of individuals with ADHD may be impaired, although some positive aspects of ADHD have been reported.22,68,69,78-84 ADHD can also be associated with substantial economic burden for the individual, their family and societal healthcare services.85,86
UNDERSTANDING ADHD: RECOGNIZING THE SIGNS AND SYMPTOMS
Date of preparation: July 2025; Job code: C-ANPROM/EUC/NBU/0002
Explore Burden of ADHD



Register as a healthcare professional
Registration gives you the benefit of access to all pages and assets on the site as well as update e-mails and additional information from Takeda on new education materials and events.
Register
